Inequity in Criminal Law Drives CCHR to Push for Greater Accountability for Rape, Drug Abuse and Fraud in Mental Health System
By CCHR International
The Mental Health Industry Watchdog
July 26, 2017
Until the passage of state laws in the United States making it a criminal offense for psychiatrists and psychologists to have sexual relationships with or even rape their patients, mental health professionals could operate with impunity—above the law. With studies showing that six to ten percent of psychiatrists, for example, acknowledge sexual involvement with their patients, that’s a potential 4,700 offenders in the U.S. alone. The Citizens Commission on Human Rights (CCHR) pressed for these laws in alignment with its founding Mental Health Declaration of Human Rights that has formed the basis of its work since 1969. The Declaration states that people have “the right to take criminal action, with the full assistance of law enforcement agents, against any psychiatrist, psychologist or hospital staff for any abuse, false imprisonment, assault from treatment, sexual abuse or rape, or any violation of mental health or other law.”
There are now 26 U.S. states that have criminalized various aspects of psychiatrist, psychologist and psychotherapist sexual contact with patients.[1]Of a sample of 120 mental health practitioners convicted for sexual crimes in the U.S., including possession of child pornography and assault of patients, more than two-thirds of the offenders were in states that have enacted such statutes. CCHR documented at least 17 cases in California, with Michigan the next highest with 12, New York at 10, Wisconsin with eight and Texas with six. Shockingly, some of the sexual assaults in the sample were against children as young as nine years old and one was even against a 4 year old. Still, that’s not surprising given a national study of therapist-client sex involving minors that revealed therapists had abused girls as young as three and boys as young as seven.[2]
Psychiatrists and psychologists rarely refer to their acts of rape as rape. Instead, they redefine this as “crossing the boundaries” when members sexually assault their patients, often with the help of drugs. In a U.S. survey of psychiatrist-patient sex, 73 percent of psychiatrists who admitted they had sexual contact with their patients claimed it was committed in the name of “love” or “pleasure;” 19 percent said it was, for example, to “enhance the patient’s self-esteem,” provide a “restitutive [compensatory] emotional experience for the patient,” while other excuses included “judgment lapse,” “therapist enhancement” and “personal needs.”[3]

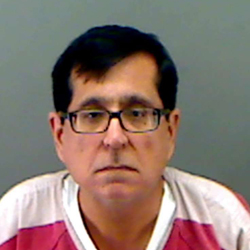
Dr. Charles “Chuck” Fischer was indicted on multiple charges of sexual assault and indecency with a child in 2012.
Dr. Charles “Chuck” Fischer was indicted on multiple charges of sexual assault and indecency with a child in 2012. For his trial Fischer paid roughly $65,000 to two psychologists whose testimony claimed a possibility that the allegations against the psychiatrist were false—the result of the accusers being mentally ill.[4]
However, prosecutors said the victims who were being treated by Fischer at the Austin State Hospital, Texas, had been taken into the psychiatrist’s office for therapy where they were molested instead. While on bail for these charges in 2013, Fischer was further arrested for public lewdness with another man.[5] On November 16, 2016, the psychiatrist was found guilty of multiple abuse charges, including four counts of sexual assault. One of his accusers said he was aged seven or eight at the time of the assault.[6]
Psychiatrists invent the most astounding excuses for their own crimes that wouldn’t see a day in court if used by a lay rapist. There’s even a “mental illness” to describe why it’s the patient’s not the psychiatrist’s fault. A member of the American Psychiatric Association (APA), psychiatrist Richard Simons once described what he calls “Masochistic Personality Disorder” (MPD) sufferers as “patients who unconsciously provoke therapists either to give up on them, or sadistically abuse them….” Whatever the “unconscious motives may be in an individual case the final behavioral outcome is the achievement of…’victory through defeat,’ and often the defeat is failed psychiatric treatment,” Simons claimed.[7]
Similarly, Australian psychiatrist Oscar Schmalzbach argued that some women who are domestically abused bring it on themselves because they “behave in such a way likely to incite violence in their partners.” He called this the Delilah Syndrome after the biblical figures Delilah and Samson.[8] A consultant psychiatrist to the New South Wales Attorney General’s department, Schmalzbach turned-up at an Australian-Asian Pacific Forensic Science Congress in August 1982 with a paper titled, “Evil in Women – ‘Delilah Syndrome’ – A New Psychiatric Syndrome.” The symptoms included pathological lying; manipulating the environment by creating tension in a domestic situation; and replacing one Samson with another.
Schmalzbach claimed: “Any amount of resentment created by some women denying the existence of the ‘Delilah Syndrome’ contributes not to improvement but to deterioration of the serious sociological and psychiatric condition … One cannot disregard the evil aspect in some women (Delilahs). Those symptoms, if diagnosed properly, would helpfully prevent the injustice created by seeing only one side of the coin—a ‘bad man’ and closing the eye on a ‘bad women’.”[9]
Imagine a criminal court judge hearing a defense argument that, “It wasn’t really rape, more like crossing the boundaries” or it was the “victim’s fault because she suffers from Delilah Syndrome.” Worse still, imagine the rape victim was your sister, brother, daughter or son, who trustingly sought help from the psychiatrist. You would rightly want the rapist prosecuted to the full extent of the law. Unfortunately, too often when it comes to a psychiatrist or psychologist the offense is reported to professional registration board instead of to the police. Medical Board may treat it as a mere ethical hiccup. At best, the perpetrator could lose his license to practice—while never going to jail as other rapists do—or receive a temporary license suspension. Such is the inequity in the law. Meanwhile the victim may be institutionalized, become suicidal—betrayed by those who claim to help.
A 2013 article about physician sexual assault, reported that about 25 percent of doctors in the U.S. face malpractice charges every year, including lawsuits over sexual misconduct. Psychiatrists, who comprise only six percent of all doctors, account for 28 percent of all physicians disciplined for sex-related offenses.[10] Lawsuits regarding inappropriate relationships have resulted in judgments or settlements in favor of the patient ranging from $300,000 to nearly $1 million, according to one law firm.[11] In one case, the psychiatrist had been sexually involved with his patient while treating her for 26 years. The psychiatrist’s “defense” was that the woman had fabricated the sexual relationship. The case settled for $950,000.[12]
The inequity in the way therapists are held accountable for patient sexual abuse has CCHR calling for more uniform laws and greater penalties to curb such rampant sexual assault.
CCHR has worked with prosecutors for years bringing those psychiatrists and psychologists to account for sexual crimes. As one Senior District Attorney, Dennis D. Bauer, from Orange County, California, wrote CCHR: “…I have been a prosecutor for 12 years and have specialized in Sexual Assaults and Child Abuse prosecutions for the past four years. I was incredulous to find out that a private organization was following up on leads where we had drawn blanks or were unable to cover. I found all [of CCHR’s] personnel very positive, eager, intelligent and exceptionally well informed on issues that are obscure to the majority of the population.”
Psychiatrists Create Fraud
 If psychiatrists’ excuses for their sexual crimes appear ingenious in their inventiveness, their fraud schemes are even more creative.
If psychiatrists’ excuses for their sexual crimes appear ingenious in their inventiveness, their fraud schemes are even more creative.
The range of fraud committed by psychiatrists and psychologists includes billing:
- Insurers for therapy that was given to people who were dead.
- “False claims”—billing for services never rendered or delivered.
- The insurance company for patients listening to music.
- For counseling clients when they were actually in jail or hospitalized.
- For patient “wake-up” calls as therapy visits.
- For having sex with patients.
- For having patients watch movies.
The insurance company Blue Cross & Blue Shield United of Wisconsin once reported that there are as many types of health insurance fraud as “the criminal mind can invent.”[13] In 1992, Texas State Senator Mike Moncrief described such fraud: “…[W]e have uncovered some of the most elaborate, creative, deceptive, immoral, and illegal schemes being used to fill empty hospital beds…. This is not just unreasonable. It is outrageous. And it is fraudulent.”[14] He was referring to a private-for-profit psychiatric hospital chain, Psychiatric Institutes of America owned by National Medical Enterprises (NME). NME offered up to $2,000 in referral or “bounty hunter fees” for referring patients to its psychiatric facilities.[15] On August 26, 1993, the FBI and other federal U.S. agencies that had been investigating health care facilities raided NME, resulting in the company paying out $575 million in settlements.[16]
CCHR was in the forefront of the campaign exposing massive psychiatric fraud committed at NME facilities, providing evidence to the FBI and other Federal and state agencies. Laws were subsequently passed outlawing psychiatric hospital bounty-hunting. CCHR representatives also met with NME executives following the Federal raids as well as with U.S. Department of Justice (DOJ) officials to discuss the curbing of psychiatrists’ fraud. In January 1994, NME announced to investors that it was dumping its psychiatric division, with its chairman stating this “signals our resolve to exit the psychiatric business.”
Since then, and including NME’s fines, CCHR has documented over $3.7 billion in criminal and civil fraud settlements and fines in the private for-profit psychiatric hospital sector.
Healthcare fraud generally costs the U.S. an estimated $100 billion a year.[17] In November 2015, Psychiatric Times reported an estimation of between 10 and 20 percent of state mental health funds alone—$4 to $8 billion—are being lost to fraud, waste, and excess profits to for-profit managed care companies. For Medicaid and Medicare fraud carried out by mental health providers, one study identified almost $1 billion in false claims reported in 2014. The article cited the case of a psychiatrist at a mental health center in Miami who was convicted for being part of a $55 million Medicare fraud; he was sentenced to 12 years in prison.[18]
Richard Kusserow, a former 11-year U.S. Department of Health and Human Services Inspector General, pointed out in 2014 that “Many health care fraud investigators believe mental health caregivers, such as psychiatrists and psychologists, have the worst fraud record of all medical disciplines.”[19]
A study published in the BJPsych Bulletin in 2014 also discussed how “no other health specialty attracts” such a “hugely negative portrayal” as psychiatrists, including media reporting that psychiatrists are out to harm, manipulate or “defraud us of our money?”[20] But the evidence supports this.
-
Houston psychiatrist Riaz Mazcuri was convicted by a federal jury of one count of conspiracy to commit healthcare fraud and five counts of fraud relating to his involvement with a $158 million Medicare fraud scheme that run out of Riverside General Hospital.
In May 2017, Houston psychiatrist Riaz Mazcuri was convicted by a federal jury of one count of conspiracy to commit healthcare fraud and five counts of fraud relating to his involvement with a $158 million Medicare fraud scheme that run out of Riverside General Hospital. Bribes and kickbacks were paid to nursing homes and group homes in exchange for sending people to Riverside. Mazcuri filed more than $4.5 million in fraudulent service claims on behalf of himself and another $55 million through Riverside hospital.[21]
- In May 2015, psychologist Sharon A. Rinaldi, 60, pleaded guilty to defrauding Medicare as part of a nationwide fraud strike force takedown. Rinaldi was charged with submitting false claims to Medicare, according to a statement from the U.S. attorney’s office. This included billing for providing services to patients that were dead, for treating patients on days when she was on trips to Las Vegas and San Diego and inflating the number of hours that she had provided services, sometimes exceeding more than 24 hours in a single day, prosecutors said. In total, she submitted false claims totaling more than $1.1 million and was reimbursed at least $447,155 by Medicare in funds to which she was not entitled.[22] In 2016, she turned herself in to the Alderson Federal Prison Camp in West Virginia to begin serving a 15-month sentence stemming from her conviction.[23]
Today, the FBI, Health and Human Services-Office of Inspector General and the U.S. attorney’s office devote vast resources to investigate, catch and prosecute those committing health care fraud.[24]
U.S. Government Creates Protection against Fraud
- In 1977, the United States Congress recognized that fraud was occurring in the Medicaid program and that special investigative/prosecution units were required. As a result, legislation was passed providing for the establishment of state Medicaid Fraud Control units.
- In 1978, the Office of Attorney General created a Medicaid Fraud Control Unit, and it was certified by the Federal government the same year. In 1986, it became the Health Care Fraud Division of the Attorney General’s office.[25]
- According to the DOJ, “the Health Insurance Portability and Accountability Act of 1996 (HIPAA) established a national Health Care Fraud and Abuse Control Program (HCFAC) under the joint direction of the Attorney General and the Secretary of the Department of Health and Human Services (HHS), designed to coordinate Federal, state and local law enforcement activities with respect to health care fraud and abuse.”[26]
- In 2009 the Health Care Fraud Prevention & Enforcement Action Team (HEAT), an initiative that combined increased tools and resources, was formed. HEAT is comprised of top level law enforcement agents, prosecutors, attorneys, auditors, evaluators, and other staff from DOJ, HHS, and their operating divisions, and is dedicated to joint efforts across government to both prevent fraud and enforce current anti-fraud laws around the country.[27]
Since 2014, CCHR’s investigations are into several large chains of behavioral facilities include those owned by Acadia Healthcare, Tenet Healthcare and Universal Health Services (UHS), the latter under U.S. Federal DOJ investigation for potential billing fraud in 26 of its facilities.[28]
In June 2017, former U.S. Congressman Ronnie Shows writing in The Daily Caller suggested that to address wasteful healthcare spending, the government could eliminate fraud and abuse. According to one government analysis, he said, Medicare fraud costs the American taxpayer over $50 billion dollars a year. And last year the Department of Health and Human Services stated that improper payments under Medicaid accounted for over 10 percent of total Medicaid spending —$139 billion dollars. “Sadly, when it comes to healthcare fraud, mental health and drug treatment programs are some of the worst actors,” Shows wrote. One company with a problematic record, he said, was Psychiatric Solutions Inc. (PSI). A shareholder lawsuit filed against PSI in 2009 alleged abuse, neglect and even death of patients. In 2010, UHS purchased PSI, accepting its legal liabilities. UHS settled the lawsuit for $65 million in 2015. “Now, UHS has more than 200 psychiatric facilities across the country and more than a third of the company’s $7.5 billion annual revenue comes from Medicare and Medicaid,” Shows added. Notably, after PSI was acquired by UHS in 2010, most of its executive team moved to Acadia Healthcare, the article continues. Of the seven individuals Acadia lists as the senior management team, all but one previously worked at or with PSI. Shows commented, “I am singling out PSI, UHS and Acadia, because they’ve received media attention, but there are many more bad actors.”[29]
Psychiatric Drugs Destroy Lives
Psychiatrists involved in trafficking of or prescribing controlled substances and prescription psychotropic drugs leading to patient overdoses or deaths are also being held criminally accountable. In reviewing a sample of 42 psychiatrists and psychologists in the past year and a half that were convicted for crimes, CCHR found nearly 20 percent (7) were for drug-related offenses. Essentially, psychiatrists destroy lives with their reliance upon prescribing mind-altering drugs, with serious adverse effects.

French psychiatrist, Daniele Canarelli, found guilty of manslaughter and sentenced to a one year suspended prison sentence after her patient, Joël Gaillard, killed a man with an axe.
Those psychiatrists being held accountable for what their patients do while under the influence of these drugs, is telling. For example, there was a 2012 conviction of French psychiatrist, Daniele Canarelli, found guilty of manslaughter and sentenced to a one year suspended prison sentence after her patient, Joël Gaillard, killed a man with an axe.[30]Charges outlined in the court judgment said the four years of the psychiatrist’s treatment of Gaillard were marked “beyond any doubt” with “a succession of failures” and her attitude “resembled blindness.” She “did not question her methodology or change her approach, thus creating or helping to create the situation that led to the realization of the crime.”[31]
In 1981, the Pennsylvania Superior Court upheld the sentence of Dr. James F. Youngkin, who was convicted of involuntary manslaughter in the death of a teenage girl to whom he had prescribed the drug Tuinal—a barbiturate, the strongest of psychotropic drugs. He was sentenced to one to three years in jail and fined $5,000. In rejecting his appeal the court ruled that “a defendant’s acts need not be the direct cause of death for criminal responsibility to be imposed.” The victim, Barbara Fedder, 17, had collapsed at a party in July 1976 and died the following day. Cause of death was ruled asphyxiation because the drug depressed her gag reflex so when she vomited, the contents went into her lungs. Trial evidence showed Dr. Youngkin issued Fedder seven prescriptions for double strength Tuinal in a two-month period. The court determined ‘‘a prescription practice that was decidedly reckless and dangerous and led, ultimately, to Ms. Fedder’s demise.’’[32]

Georgia psychiatrist, Narendra Nagareddy, 57, known as “Dr. Death,” was arrested in January 2016 after 36 of his patients died, 12 of whom passed away due to overdose on his prescription drugs.
Georgia psychiatrist, Narendra Nagareddy, 57, known as “Dr. Death,” was arrested in January 2016 after 36 of his patients died, 12 of whom passed away due to overdose on his prescription drugs.[33] Clayton County Police Chief Mike Register told media that the psychiatrist had been “overprescribing opiates and benzodiazepines” and there had been “a multitude of overdoses and overdose deaths.”[34] The case involves three victims aged between 29 and 49. One, Audrey Austin, 29, filled several prescriptions from Nagareddy on February 20, 2014, for alprazolam, a generic version of the sedative hypnotic, Xanax, and methadone tablets. The next day, she filled a prescription issued from Nagareddy for amphetamine and died later that day from a prescription overdose, according to a warrant.[35] The psychiatrist is currently under house arrest, pending his trial, tracked via an ankle monitor.[36]
The point being, psychiatrists are trained in medical procedures and are fully aware of the effects of these drugs and potentially lethal consequences that others may not be aware of.
Psychiatric Ghost Writing Generates Suicide?
Where psychiatrists and researchers put their names to medical studies they have not written but, instead, have been written by Public Relations/Marketing pros and those studies withhold information about serious risks that could harm consumers, those researchers should be subject to charges of professional misconduct and fraud.[37] Any damage to the consumer that may occur as a result of the misrepresentation should be subject to criminal and civil recourse.
 Consider what is known as “Study 329,” regarding GlaxoSmithKline’s (GSK) antidepressant Paxil (paroxetine) published in 2001 in the Journal of the American Academy of Child and Adolescent Psychiatry. 329 was cited in a lawsuit brought by the New York Attorney General in 2004 charging GSK with ‘‘repeated and persistent fraud’’ for promoting positive findings and not publicizing unfavorable data—that the drug could increase the risk of suicide in children prescribed the drug. The suicide risk ratio for adolescents exposed to Paxil in Study 329 was six times greater than those on placebo.[38]
Consider what is known as “Study 329,” regarding GlaxoSmithKline’s (GSK) antidepressant Paxil (paroxetine) published in 2001 in the Journal of the American Academy of Child and Adolescent Psychiatry. 329 was cited in a lawsuit brought by the New York Attorney General in 2004 charging GSK with ‘‘repeated and persistent fraud’’ for promoting positive findings and not publicizing unfavorable data—that the drug could increase the risk of suicide in children prescribed the drug. The suicide risk ratio for adolescents exposed to Paxil in Study 329 was six times greater than those on placebo.[38]
But what of the research psychiatrists that put their name to the ghost-written study? While GSK paid $2.5 million to settle the suit, none of the influential child psychiatrists listed as authors and funded by GSK were held accountable.[39] An August 2012 article in the Chronicle of Higher Education revealed that the academics who agreed to let their names be used had repeatedly ignored calls to retract the disgraced article.[40]However, as the study did not use federal funds, federal prosecutors did not have the authority to sanction the researchers.[41]
Eighteen of the Paxil study’s 22 authors were university scholars, including its lead author, Martin B. Keller and Dr. Karen Wagner who both have extensive ties to the drug industry.[42] Wagner is also a columnist for Psychiatric Times and President-Elect to the American Academy of Child and Adolescent Psychiatry.[43] She asserted, “The results of this study demonstrate the safety of paroxetine in the treatment of adolescent depression. Side effects were modest with paroxetine.” But internal GSK emails showed the data from pediatric Paxil trials were negative.[44]
Leemon McHenry, a bioethicist and a lecturer in philosophy at California State University, Northridge, co-wrote the article “Clinical Trials and Drug Promotion: Selective Reporting of Study 329.”[45] In an interview with CCHR documentary directors, he said, “Dr. Keller in this case is the first author on the paper and he’s the principal investigator in the trial. So, as an academic and as a clinical scientist, he has primary responsibility for the way in which the data is reported in the paper. However, in Keller’s deposition, he admits that he did not look at the raw data.” Despite Study 329 having been “determined to be fraudulent” he added, the Keller study “is frequently cited as the main source of evidence for the effectiveness and safety of Paxil for children and adolescents.”
“Many, many children and adolescents were put on this drug and became suicidal and some of them did in fact commit suicide on the drug,” McHenry continued. How many more continue to do so in the belief that the drug is “safe” and adverse effects are merely “modest”?
Attorney Stephen Sheller has won numerous cases involving the danger of the antipsychotic drug, Risperdal (risperidone). In discussing misleading articles, he said he once had to threaten to sue a doctor who knew the data in his article was misleading and false and doctors were relying on it. “He’s been given an opportunity to correct it. If he doesn’t and I find a doctor who prescribed the drug to one of my clients, based on reliance on that article, he will be sued. That’s what you got to do.”
The Guardian in the UK reported that legal experts have called for severe sanctions against scientists who ‘guest author’ papers written by drug companies. As the article stated, “In the worst cases, doctors receive payments or other incentives to endorse articles without being familiar with the studies or data the reports describe. Often, the articles are biased and do not carry the names of the real authors.”[46]
Writing in the journal PLoS Medicine, Simon Stern and Trudo Lemmens, both law professors at the University of Toronto, said: “We argue that a guest author’s claim for credit of an article written by someone else constitutes legal fraud, and may give rise to claims that could be pursued in a class action based on the Racketeer Influenced and Corrupt Organizations Act (RICO)” in the U.S.[47] Lemmens added: “It’s a prostitution of their academic standing. And it undermines the integrity of the entire academic publication system.”[48]
Victims Sue Psychiatric Practices
 According to Professional Risk Management Services, Inc., which has managed more lawsuits, claims and potential claims against psychiatrists than any other professional liability insurance program in the U.S., the two top liability risks for psychiatrists are “patients with suicidal behavior and psychopharmacology.” While patient suicides may trigger the most lawsuits, cases with the largest verdicts or settlements involve permanent physical and neurological damage requiring lifelong care. For example, damage from renal failure from lithium toxicity.[49]
According to Professional Risk Management Services, Inc., which has managed more lawsuits, claims and potential claims against psychiatrists than any other professional liability insurance program in the U.S., the two top liability risks for psychiatrists are “patients with suicidal behavior and psychopharmacology.” While patient suicides may trigger the most lawsuits, cases with the largest verdicts or settlements involve permanent physical and neurological damage requiring lifelong care. For example, damage from renal failure from lithium toxicity.[49]
Psychiatric malpractice lawsuits frequently include allegations of negligence related to the prescription of psychotropic drugs.[50] Many psychiatric drugs are well documented to cause suicidal and violent behavior. Inappropriate prescriptions for patients are another source of legal difficulty for psychiatrists.[51] One study found inappropriate prescribing for patients represented 11 percent of legal complaints against physicians.[52]
An International Journal of Law & Psychiatry study found that 43 percent of legal complaints against psychiatrists involved patient suicide or attempted suicide.[53]
Psychiatric Schools, Colleges, Associations
It would behoove attorneys to look at who else should be held accountable for the extensive level of abuse and fraud that passes for psychiatric therapy today. Take, for example, the chemical imbalance theory promoted as a source of depression, or the spurious claim that there is a genetic link to Attention Deficit Hyperactivity Disorder (ADHD). More than a decade after CCHR was exposing that the chemical imbalance theory was a lie, Dr. Ronald Pies, editor-in-chief emeritus of the Psychiatric Times, laid the theory to rest in the July 11, 2011 issue of the Times with this: “In truth, the ‘chemical imbalance’ notion was always a kind of urban legend — never a theory seriously propounded by well-informed psychiatrists.”[54]
Were that true, why, then, didn’t the American Psychiatric Association pound it home to its members not to defraud their patients with assertions that the chemical imbalance mantra had merit? Who were these “well-trained” psychiatrists that knew all along but apparently remained silent that the theory—leading to millions of Americans taking potentially damaging and suicide-inducing antidepressants—was a fraud? This is complicity in one of the greatest hoaxes ever committed on the American people.
And if medical schools and colleges have taught such fraud as fact, might not they equally share in the burden of responsibility? Shouldn’t lawsuits challenge their training that leads to such irresponsible practices and dangerous “standards of care”?
CCHR is calling on anyone whose family member or friend has been the victim of dangerous psychiatric drug prescription practices or electroshock and other brain-intervention psychiatric therapies; sexual assault, billing fraud, negligence or any other crime or abuse committed in the mental health system to contact CCHR. Submit your report of psychiatric abuse here.
States that have Criminalized Sexual Relationships between Psychotherapists and Patients
Alaska, Arizona, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Iowa, Kansas, Maine, Maryland, Michigan, Minnesota, Mississippi, New Hampshire, New Mexico, New York, North Dakota, Ohio, South Dakota, Texas, Utah, Washington, and Wisconsin.[55] The New York state criminal code also says therapists, counselors, psychologists and psychiatrists are guilty of statutory rape if they have sex with patients during the course of a treatment session.[56]
For references, click HERE.


